Filter
220
Featured
67
Language
Document type
123
42
23
8
7
6
5
2
2
2
Countries / Regions
30
23
14
11
8
8
8
8
7
6
6
5
5
4
4
4
4
3
3
3
3
2
2
2
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
Authors & Publishers
Publication Years
Category
117
18
9
4
1
1
As of 12 December 2022, over 645 million people worldwide have been diagnosed with COVID-19, with over 6.6 million deaths (4).
The Omicron variant, which emerged in late November 2021, and its subvariants, are now the dominant circulating viruses, contributing to the ongoing surge in several countr
...
The WHO continuously reviews available data on SARS-CoV-2 variants of concern. For this version, the global epidemiological
situation of the COVID-19 pandemic as of 21 January 2022 – at a time when the Omicron VOC had been identified in 171
countries across all six WHO Regions and was rapidly re
...
The WHO COVID-19 Clinical management: living guidance contains the most up-to-date recommendations for the clinical management of people with COVID-19. Providing guidance that is comprehensive and holistic for the optimal care of COVID-19 patients throughout their entire illness is important.
WHO has updated its guidelines for COVID-19 therapeutics, with revised recommendations for patients with non-severe COVID-19. This is the 13th update to these guidelines.
Updated risk rates for hospital admission in patients with non-severe COVID-19
The guidance includes updated risk rates for
...
First published in 2020, this toolkit is intended for clinicians working in acute care, managing adult and paediatric patients with acute respiratory infection, including severe pneumonia, acute respiratory distress syndrome, sepsis and septic shock. The main objective is to provide key tools for us
...
The WHO COVID-19 Clinical management: living guidance contains the Organization’s most up-to-date recommendations for the clinical management of people with COVID-19. Providing guidance that is comprehensive and holistic for the optimal care of COVID-19 patients throughout their entire illness is
...
Updated 2022. This guide addresses the care pathway from presentation of the patient to a health facility to patient discharge. It considers different levels of disease severity, from asymptomatic individuals to critically ill patients. Accounting for variations in the benefits and harms of chest im
...
Ce document d'orientation est destiné aux cliniciens qui s'occupent de patients atteints de COVID-19 à toutes les phases de leur maladie (c'est-à-dire du dépistage à la sortie de l'hôpital). Cette mise à jour a été étendue pour répondre aux besoins des cliniciens de première ligne et fa
...
This twelfth version of the WHO living guideline now contains 19 recommendations. This latest update provides updated recommendations for remdesivir, addresses the use of combination therapy with corticosteroids, interleukin-6 (IL-6) receptor blockers and Janus kinase (JAK) inhibitors in patients wi
...
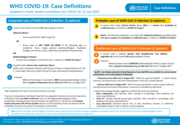
22 July 2022. This document provides the case definitions for public health surveillance of COVID-19 in humans caused by SARS-COV-2 infection.
3 March 2022
The WHO Therapeutics and COVID-19: living guideline contains the Organization’s most up-to-date recommendations for the use of therapeutics in the treatment of COVID-19. The latest version of this living guideline is available in pdf format (via the ‘Download’ button) and via an
...
Poster, 4 Janaury 2022
Updated Treatment Guidelines
The COVID-19 CARE pathway is a living tool to support health care workers visualize the current clinical and therapeutic recommendations to be considered in the care planning for patients with COVID-19.
The COVID-19 CARE pathway is aligned with the eighth version of the WHO Therapeutics and COVID
...
The COVID-19 CARE pathway is a living tool to support health care workers visualize the current clinical and therapeutic recommendations to be considered in the care planning for patients with COVID-19.
The COVID-19 CARE pathway is aligned with the eighth version of the WHO Therapeutics and COVID
...
Ongoing Living Update of COVID-19 Therapeutic Options: Summary of Evidence, Rapid Review 22 February 2022
recommended
This document includes the results of a rapid systematic review of current available literature. The information included in this review reflects the evidence as of the date posted in the document. In recognition of the fact that there are numerous ongoing clinical studies, PAHO will periodically up
...
List of essential medicines for the management of patients admitted in intensive care units with a suspected or confirmed diagnosis of COVID 19. Third version, 1 February 2022
26 de abril del 2022. La Organización Panamericana de la Salud presenta estas consideraciones con el fin de apoyar la toma de decisiones relativa al manejo de pacientes con COVID-19 en la Región de las Américas. Las recomendaciones tienen en cuenta la evidencia más reciente, el estado de vacunac
...