Filter
8280
Text search:
control
guidelines
Featured
866
2108
Language
7165
656
341
195
129
121
45
44
32
14
13
12
11
11
9
9
7
7
7
7
6
6
6
6
6
5
5
5
5
4
4
4
4
4
4
4
4
3
3
3
3
3
3
3
2
2
2
2
2
2
2
2
1
1
1
1
1
1
1
1
1
1
1
1
1
1
Document type
4114
1648
1137
553
343
173
169
60
29
19
19
6
5
2
1
Countries / Regions
429
347
237
186
172
153
152
152
149
148
134
125
121
118
110
104
103
94
88
77
76
75
72
70
68
67
67
61
59
59
52
51
48
47
46
46
44
43
42
42
42
41
40
38
38
35
33
32
32
31
30
29
28
27
26
26
24
19
19
16
16
15
15
15
14
13
13
12
12
11
11
11
10
10
10
9
9
9
9
8
8
8
8
7
7
7
7
6
6
6
6
5
5
5
5
5
5
5
4
4
4
4
4
4
4
3
3
3
3
3
3
3
3
3
3
3
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
Authors & Publishers
1109
381
301
215
189
132
127
118
84
79
67
57
55
52
49
45
40
39
38
36
35
34
34
30
30
29
29
28
28
27
27
27
25
25
24
23
23
23
23
23
23
22
22
22
22
22
21
20
20
20
19
19
19
19
18
18
18
18
18
18
17
17
17
17
16
16
15
15
15
15
14
14
14
14
14
14
14
14
13
13
13
13
13
13
13
13
12
12
12
12
12
12
12
12
12
12
11
11
11
11
11
11
11
11
10
10
10
10
10
10
10
10
10
10
10
10
9
9
9
9
9
9
9
9
9
9
9
9
9
9
9
9
9
9
9
8
8
8
8
8
8
8
8
8
8
8
8
8
8
7
7
7
7
7
7
7
7
7
7
7
7
7
7
7
7
7
7
7
7
7
7
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
6
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
5
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
4
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
3
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
Publication Years
1
2547
4912
773
45
1
1
Category
3412
694
569
464
395
160
116
2
Toolboxes
851
613
549
443
315
288
253
227
204
199
174
168
157
152
143
119
118
100
91
85
79
51
45
42
20
1
A aplicação da tecnologia digital de saúde está crescendo rapidamente na África, com o
objetivo de melhorar a prestação de serviços de saúde e alcançar de forma mais eficaz
comunidades remotas e carentes. A falta de diretrizes e padrões habilitadores em todo o
continente, por outro
...
lado, dificulta o compartilhamento de dados de forma significativa em
todo o continente. Considerando isso, os Centros Africanos de Controle e Prevenção de
Doenças (CDC África) estabeleceram uma força-tarefa de 24 membros para fornecer
experiência e orientação no desenvolvimento de diretrizes e padrões da AU HIE. Os membros
da força-tarefa eram especialistas no assunto que trabalhavam na África e
internacionalmente na coleta, análise e troca de informações de saúde. Alguns desses
especialistas estiveram envolvidos em consultas anteriores sobre a definição da estratégia de
sistemas de informação de saúde do CDC África. Um presidente, copresidente e secretário
foram eleitos para envolver os membros da força-tarefa em diferentes grupos de trabalho
técnicos.
more
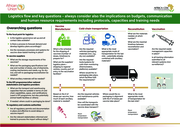
Este manual está dirigido al personal de salud que trabaja en establecimientos periféricos y que utiliza pruebas de diagnóstico rápido (PDR) para la malaria. Proporciona instrucciones prácticas para garantizar el buen funcionamiento de estas pruebas en condiciones muchas veces difíciles, espec
...
ialmente en zonas remotas y de clima cálido.
Se explican procedimientos clave para la recepción de las pruebas (verificación de daños, caducidad, condiciones de transporte), el almacenamiento (selección del lugar más fresco, control de temperatura, ventilación, uso de métodos sencillos como depósitos en el suelo o contenedores que enfrían por evaporación) y el transporte seguro, ya sea por tierra o agua, con especial atención a evitar la exposición al calor.
Además, el manual incluye pautas para la gestión de inventarios, la rotación de existencias (usando primero las pruebas con vencimiento más próximo), y el registro del uso para evitar desperdicios y asegurar la disponibilidad continua.
Finalmente, se aborda la gestión de desechos peligrosos y generales generados por el uso de las pruebas, promoviendo su separación adecuada, almacenamiento seguro y eliminación apropiada (como fosas protegidas o incineración controlada), con el fin de proteger al personal y a la comunidad.
more
18 Janaury 2021
EU/EEA Member States and the UK have increased their laboratory capacity tremendously over the past 11 months as the majority of the Member States reported sufficient testing capacity until March 2021.
Many countries are adding rapid antigen detection tests (RADT) to their
...
testing strategies in order to reduce pressure on RT-PCR testing.
Some Member States have already included RADT in their case definition.
The main bottlenecks, such as shortages of laboratory consumables and human resources, as well as sample storing facilities, continue to exist and may affect the overall laboratory response to COVID-19.
more
This toolkit is a "how to" guide for developing, implementing and evaluating a multisectoral action plan for prevention and control of NCDs. It is targeted at policy-makers, planners and programme managers, and is intended to help countries, provinc
...
es and cities meet the requirements for achieving global and national NCD targets and the Sustainable Development Goals. The toolkit takes the user through a series of actions related to the development of a multisectoral action plan ("MSAP development actions"), and provides forms and a template framework for users to complete as they undertake these actions. Developing a multisectoral action plan involves establishing health needs and engaging relevant stakeholders before determining the actions to take, identifying and prioritizing interventions, deciding on ways to address NCDs while establishing support and resources for prevention and control, and evaluating progress in implementing the plan.
more
This toolkit is a "how to" guide for developing, implementing and evaluating a multisectoral action plan for prevention and control of NCDs. It is targeted at policy-makers, planners and programme managers, and is intended to help countries, provinc
...
es and cities meet the requirements for achieving global and national NCD targets and the Sustainable Development Goals. The toolkit takes the user through a series of actions related to the development of a multisectoral action plan ("MSAP development actions"), and provides forms and a template framework for users to complete as they undertake these actions. Developing a multisectoral action plan involves establishing health needs and engaging relevant stakeholders before determining the actions to take, identifying and prioritizing interventions, deciding on ways to address NCDs while establishing support and resources for prevention and control, and evaluating progress in implementing the plan.
more
The article "Malaria – MSD Manual Professional Edition" provides a comprehensive overview of malaria, an infection caused by Plasmodium species. It describes symptoms such as fever, chills, and anemia, explains diagnostic methods like parasite detection in blood smears, and discusses treatment opt
...
ions including artemisinin-based combination therapies. In addition, it outlines prevention strategies such as medical prophylaxis and mosquito control measures. The article is intended for medical professionals and offers detailed information on the pathophysiology, clinical presentation, and management of malaria.
more
The document titled "Checklist for Assessing Management of Severe Malaria" is part of the MalariaCare Toolkit. It provides a structured tool for supervisors conducting outreach training and supportive supervision (OTSS) visits in healthcare facilities. The checklist is designed to evaluate and guide
...
the clinical management of severe malaria cases, including diagnostics, treatment planning, complication management, patient monitoring, and the administration of injectable artesunate. It also includes sections for direct observation of clinical procedures and supervisor feedback to help improve healthcare worker performance and adherence to national treatment guidelines.
more
Las Directrices de la OMS sobre la malaria reúnen las recomendaciones más actualizadas de la Organización acerca de la malaria (o paludismo) en una plataforma en línea fácil de usar y de navegar.
La primera versión de las Directrices es una recopilación de las recomendaciones existentes de
...
la OMS sobre la malaria y reemplaza a dos publicaciones anteriores de la OMS: las Directrices para el tratamiento del paludismo, tercera edición (en inglés unicamente), y las Directrices para el control de vectores del paludismo. Se seguirán revisando las recomendaciones sobre la malaria y, cuando proceda, se actualizarán en función de los últimos datos probatorios disponibles. Todas las recomendaciones actualizadas mostrarán siempre la fecha de la revisión más reciente en la plataforma MAGICapp. Con cada actualización, habrá también disponible en el sitio web de la OMS una nueva versión en PDF de las directrices unificadas que se podrá descargar.
Esta versión corresponde a la publicada en inglés el 13 de julio del 2021. La actualización se está traduciendo actualmente.
more
The "Integrated Management of Malaria Training – Health Worker’s Manual" is a practical guide developed by Uganda’s Ministry of Health to train healthcare workers at all levels in the effective diagnosis, treatment, prevention, and management of malaria. It aligns with national malaria treatme
...
nt guidelines and aims to improve the quality of care and reduce malaria-related illness and death. The manual covers key topics such as clinical assessment of fever, use of rapid diagnostic tests (RDTs), case management of uncomplicated and severe malaria, malaria in pregnancy, co-infections like HIV, as well as community engagement and proper documentation. It includes structured training sessions, case studies, and job aids designed to strengthen the skills of health workers in both public and private sectors, and to ensure standardized, evidence-based malaria care across the country.
more
These pages contain links to critical guidelines, technical documents, tools and resources needed to investigate and respond to outbreaks.
Available in Englisch, French, Spanish and Chinese
The document provides guidelines for the management of acute diarrhoea, highlighting improved oral rehydration solutions (ORS) with reduced osmolarity and zinc supplementation. It emphasizes their
...
effectiveness in reducing the duration and severity of diarrhoeal episodes and preventing future cases. Aimed at families, communities, and healthcare professionals, it seeks to integrate these practices into routine care at home and in health centers.
more
Quality Assurance Framework for SARS-CoV-2 Antigen Rapid Testing for Diagnosis of COVID-19
recommended
ASLM in collaboration with the Africa Centres for Disease Control and Prevention, and in partnership with the Clinton Health Access Initiative, Amref and Last Mile Health present the Quality Assurance Framework for SARS-CoV-2 Antigen Rapid Testing f
...
or Diagnosis of COVID-19. This framework aims to provide general technical guidance to African Union Members States on the rollout, establishment, implementation, monitoring, and evaluation of SARS-CoV-2 Ag RDT interventions so as to effectively and efficiently detect, control and minimise errors in the performance of COVID-19 laboratory testing processes. It describes the core components for quality assurance, resources mobilisation and advocacy for scale up, monitoring, evaluation, learning and accountability for SARS-CoV-2 implementation.
more
ASLM in collaboration with the Africa Centres for Disease Control and Prevention, and in partnership with the Clinton Health Access Initiative, Amref and Last Mile Health present the Quality Assurance Framework for SARS-CoV-2 Antigen Rapid Testing f
...
or Diagnosis of COVID-19. This framework aims to provide general technical guidance to African Union Members States on the rollout, establishment, implementation, monitoring, and evaluation of SARS-CoV-2 Ag RDT interventions so as to effectively and efficiently detect, control and minimise errors in the performance of COVID-19 laboratory testing processes. It describes the core components for quality assurance, resources mobilisation and advocacy for scale up, monitoring, evaluation, learning and accountability for SARS-CoV-2 implementation.
more
“Guide to facilitate the implementation of the WHO/UNICEF “Guidance on developing a national deployment and vaccination plan for COVID-19 vaccines” for Africa
This guidance covers diagnosis and care of patients with long-term effects of COVID-19. It makes recommendations for the care of adults and children who have new or ongoing symptoms 4 weeks or more after the start of acute COVID-19. It is meant for health and care practitioners. This interim documen
...
t has been developed by the Africa Taskforce on Coronavirus Case Management Technical Working Group and will be continuously reviewed and updated in response to emerging evidence
more
27 May 2021
This is a document to support the use of pulse oximeter for assessment of suspected and confirmed cases of Covid-19 in the community.
It is a well-known fact that Covid-19 can present as “happy hypoxia” with minimum symptoms of severe respiratory distress despite significant low ox
...
ygen levels in the blood. The use of pulse oximeter for clinical assessment significantly augments decision making, save lives and provide high quality care. It allows for early detection of patients with hypoxia requiring either close monitoring in the community or timely referral for hospital care.
more
The World Health Organization provides regional and national strategies and operational plans that aim to support countries in work to achieve measles control and elimination. These are guided by high level frameworks including the Immunization Agen
...
da 2030 and the Measles and Rubella Strategic Framework 2021–2030. These frameworks promote improvements in routine immunization programmes to reach all children, reduce immunity gaps and prevent outbreaks within the context of universal health care.
This interim guidance on Targeted and selective strategies in measles and rubella vaccination campaigns adds to the suite of guidance documents. It provides expanded description of methods to determine age groups for inclusion in preventive and outbreak response measles and rubella vaccination campaigns; and operational considerations that are specific to targeted and selective strategies in measles and rubella vaccination campaigns. This guidance also updates definitions for tailored, targeted and selective campaigns.The World Health Organization provides regional and national strategies and operational plans that aim to support countries in work to achieve measles control and elimination. These are guided by high level frameworks including the Immunization Agenda 2030 and the Measles and Rubella Strategic Framework 2021–2030. These frameworks promote improvements in routine immunization programmes to reach all children, reduce immunity gaps and prevent outbreaks within the context of universal health care.
This interim guidance on Targeted and selective strategies in measles and rubella vaccination campaigns adds to the suite of guidance documents. It provides expanded description of methods to determine age groups for inclusion in preventive and outbreak response measles and rubella vaccination campaigns; and operational considerations that are specific to targeted and selective strategies in measles and rubella vaccination campaigns. This guidance also updates definitions for tailored, targeted and selective campaigns.
more
The Story of Cholera, Kannada
recommended
The Story of Cholera was produced in collaboration with award-winning animator Yoni Goodman.
This animation covers cholera transmission, prevention, signs, and care in a simple and accessible way. The film follows evidence-based guidelines, has bee
...
n field-tested, and reviewed for accuracy and content. Download flashcards and mobil phone versions from the website
more