Filter
7539
Filtered Results: 7539
Text search:
African
Health
Organisation
Featured
Recommendations
677
New Publications
1694
Language
Document type
No document type
3978
Studies & Reports
1543
Guidelines
848
Manuals
366
Strategic & Response Plan
283
Fact sheets
202
Training Material
125
Situation Updates
73
Resource Platforms
37
Infographics
27
Online Courses
23
Brochures
18
Videos
7
Dashboards/Maps
6
App
3
Countries / Regions
Global
379
Kenya
242
South Africa
240
Sierra Leone
208
Africa
207
Nigeria
187
Liberia
185
Ethiopia
172
Uganda
162
Congo, Democratic Republic of
124
Zambia
124
Malawi
121
Rwanda
117
Tanzania
114
Ghana
105
India
105
Middle East and North Africa
102
Senegal
100
West and Central Africa
97
Namibia
88
Mozambique
85
Guinea
80
South Sudan
79
Syria
77
East and Southern Africa
73
Latin America and the Carribbean
71
Western and Central Europe
70
Burkina Faso
68
Yemen
62
Lesotho
61
Zimbabwe
61
Nepal
54
Benin
47
Cameroon
47
Central African Republic
47
Bangladesh
46
Russia
39
Ukraine
38
Mali
36
Asia
34
Botswana
34
Sudan
31
South–East Asia Region
30
Brazil
30
Angola
30
Myanmar / Burma
30
Madagascar
29
Eastern Europe
27
Côte d’Ivoire / Ivory Coast
25
Somalia
25
Eswatini/ Swaziland
25
Haiti
24
China
23
Indonesia
23
Cambodia
22
Colombia
18
Philippines
18
Chad
18
Pakistan
17
Afghanistan
16
Guinea-Bissau
16
Germany
16
Togo
15
Thailand
14
Niger
13
Venezuela
12
Eastern Europe and Central Asia
12
Vietnam
12
Iraq
10
Lebanon
9
Sri Lanka
9
Iran
8
Jordan
8
Saudi Arabia
8
North America
8
Libya
8
Mexico
7
Gambia
7
Burundi
7
Southern Africa
7
Egypt
7
Western Pacific Region
6
Tunisia
6
Portugal
6
Papua New Guinea
6
Chile
5
Morocco
5
Jamaica
5
Japan
5
Argentina
5
Ecuador
5
Albania
4
Laos
4
Peru
4
Malaysia
4
Mauritania
4
Palestine
4
Georgia
4
North Macedonia
3
Serbia
3
Turkey
3
Kazakhstan
3
Kyrgyzstan
3
Qatar
3
Paraguay
3
Gabon
3
France
3
Mauritius
3
Spain
3
Israel
3
Bosnia and Herzegovina
3
Moldova
3
Djibouti
3
Greece
3
Tajikistan
2
Canada
2
Congo-Brazzaville
2
Italy
2
Armenia
2
USA
2
Turkmenistan
2
United Kingdom
2
Belarus
2
Bolivia
2
Honduras
2
North Korea
1
Timor Leste/ East Timor
1
El Salvador
1
Estonia
1
Vanuatu
1
Mongolia
1
Bulgaria
1
Dominican Republic
1
Cape Verde
1
Croatia
1
Hungary
1
Denmark
1
Belgium
1
Norway
1
South Korea
1
Algeria
1
Morocco
1
Azerbaijan
1
Eritrea
1
Nicaragua
1
Romania
1
Poland
1
Solomon Islands
1
Cuba
1
Guatemala
1
Authors & Publishers
Publication Years
Category
Countries
2572
Clinical Guidelines
585
Key Resources
412
Public Health
411
Women & Child Health
397
Capacity Building
131
Pharmacy & Technologies
84
Annual Report MEDBOX
3
Toolboxes
HIV
695
COVID-19
628
Mental Health
471
TB
432
Ebola & Marburg
368
NTDs
315
Disability
301
Planetary Health
289
Rapid Response
251
AMR
178
Caregiver
175
Global Health Education
163
Conflict
148
NCDs
140
Malaria
136
Health Financing Toolbox
135
Pharmacy
118
Refugee
116
Natural Hazards
59
Zika
57
Polio
48
Cholera
41
Social Ethics
27
Specific Hazards
22
2.0 Rapid Response
11
Typhoon
3
South Sudan
2
As a lower-middle-income country (LMIC), South Africa (SA) bears
the burden of maternal and neonatal mortality similar to other sub-
Saharan African countries. According to the Saving Mothers Report
2017/19, there has been a progressive and sustained reduction
in institutional maternal mortality...
In 2006, the Special Session of African Union Health Ministers adopted the Maputo Plan of Action for implementing the Continental Policy Framework on sexual and reproductive health and rights (SRHR), which expired at the end of 2015. The goal was for all stakeholders and partners to join forces and ...
Full Report
The application of digital health technology is growing at a rapid rate in Africa, with the goals of improving the delivery of healthcare services and more effectively reaching out to remote and underserved communities. The lack of enabling guidelines and standards across the continent, on the other...
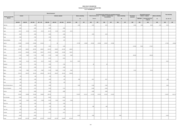
Overview on the assessed contributions for all World Health Organization Member States As at 31 December 2021.
This study aims to provide an overview of health financing in Africa and to examine the impact of the reemergence of mpox on health financing in the region.
This strategy defines the World Health Organization (WHO) vision and framework for supporting Member States to accelerate the development, implementation and monitoring of their National Action Plan for Health Security (NAPHS) from 2022 to 2026. The National Action Plan for Health Security (NAPHS) ...
Accessed Sept, 5 2018
Weekly epidemiological record, Relevé épidémiologique hebdomadaire : Vol.93 (2018) No.13
The new five-year agenda of WHO in Africa, The Africa Health Transformation Programme, 2015–2020: a vision for universal health coverage, is the strategic framework that will guide WHO’s contribution to the emerging sustainable development platform in Africa. It articulates a vision for health a...
Over the past decade, countries in the African region experienced slow progress in mobilizing resources for health while facing continued challenges. In their revised estimates published in 2017, Stenberg et al., developed two costs scenarios, termed progress and ambitious, aimed at strengthening co...
Low- and middle-income countries (LMICs) experience a high disease burden for epilepsy, a chronic neurological condition.The authors evaluate the cost-effectiveness of community health workers (CHWs) to improve adherence to medication for epilepsy in South Africa. They found that utilizing CHWs to i...
Hum Resour Health 20, 37 (2022). https://doi.org/10.1186/s12960-022-00735-y.
For countries to achieve universal health coverage, they need to have well-functioning and resilient health systems. Achieving this requires a sufficient number of qualified health workers and this necessitates the importa...
The State of the World's Midwifery
Community Health Workers in Sub Saharan Africa
recommended
A booklet on how CHWs were addressing eye health across Africa based on desk research and a survey in 23 countries