Filter
1486
Text search:
Diabetes
Therapy
Featured
174
381
Language
Document type
822
276
223
73
40
22
17
8
4
1
Countries / Regions
132
78
49
45
37
31
25
25
23
23
23
22
22
22
22
18
18
16
16
16
15
14
14
13
13
12
11
10
10
9
9
8
8
8
7
7
7
6
6
6
6
5
5
5
5
4
4
4
4
4
4
4
4
4
4
3
3
3
3
3
3
3
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
2
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
1
Authors & Publishers
Publication Years
Category
669
176
146
49
23
20
9
1
Toolboxes
191
130
111
108
54
50
39
38
37
23
14
14
13
11
8
6
6
6
5
3
3
2
1
The document provides detailed clinical guidelines for the therapy of Type 1 Diabetes as developed by the German Diabetes Association (DDG). It foc
...
Practical Guidelines of Insulin Therapy in Diabetes Mellitus Patients
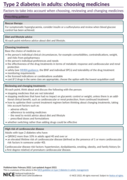
Factors to take into account when choosing, reviewing and changing medicines.
Rescue therapy:
For symptomatic hyperglycaemia, consider insulin or a sulfonylurea and review when blood glucose control has been achieved.
Diet and lifestyle advice:
...
The cardiovascular disease continuum begins with risk factors such as diabetes mellitus (DM), progresses to vasculopathy and myocardial dysfunction, and finally ends with cardiovascular death. Diabetes
...
The alarming rise in the worldwide prevalence of obesity and associated type 2 diabetes mellitus (T2DM) have reached epidemic portions. Diabetes in its many forms and T2DM have different physiologic
...
The document "Pocketbook for Management of Diabetes in Childhood and Adolescence in Under-Resourced Countries" (2nd Edition) provides practical guidelines for managing diabetes in children and adole
...
WHO guideline on HIV service delivery
recommended
Updated guidance on the integration of diabetes, hypertension and mental health services, and interventions to support adherence to antiretroviral therapy. The guideline offers practical implementa
...
Methicillin-resistant Staphylococcus aureus(MRSA) strainsor multidrug-resistant S.aureus, initially described in 1960s,emerged in the last decade as a cause of nosocomial infections responsible for rapidly progressive, potential fatal diseases including life-threatening pneumonia, necrotizing fascii
...
This study was aimed to ascertain the clinical profile and management of patients with ischemic heart disease (IHD) and/or peripheral artery disease (PAD). In this observational and cross-sectional study developed in 80 hospitals throughout Spain, consecutive adults with stable IHD and/or PAD were i
...
WHO has updated its guidelines for COVID-19 therapeutics, with revised recommendations for patients with non-severe COVID-19. This is the 13th update to these guidelines.
Updated risk rates for hospital admission in patients with non-severe COVID-19
The guidance includes updated risk rates for
...
JIMSA Jan.-March 2015 Vol. 28 no.1 p.47-50e
Since the discovery of insulin nearly 100 years ago, advances in diabetes treatments and therapies have transformed the lives of people
with diabetes (PwD), notably reducing the daily burden of its
...
The document provides quality standards for managing Type 1 diabetes in adults, emphasizing areas like structured education, continuous glucose monitoring (CGM), cardiovascular risk management, and diabetic foot assessment. It aims to improve care p
...
Guía Clínica – Diabetes Mellitus tipo 1
Erklärt ausführlich und mit Bildern was Diabetes ist, welche Formen es gibt und welche Risikosituationen auftreten können. Auch Infos zu Ernährung und Therapie-Möglichkeiten bei Diabetes sind
...
World Health Organization – Diabetes country profiles, 2016.