Filter
6141
Text search:
long-term
care
Featured
Recommendations
538
New Publications
1543
Language
Document type
No document type
3367
Studies & Reports
1109
Guidelines
799
Manuals
341
Strategic & Response Plan
249
Training Material
92
Fact sheets
90
Situation Updates
45
Brochures
19
Resource Platforms
14
Infographics
10
Online Courses
3
App
1
Countries / Regions
Global
311
India
241
Kenya
173
Nepal
132
Sierra Leone
125
South Africa
121
Western and Central Europe
115
Liberia
107
Ethiopia
106
Myanmar / Burma
100
Uganda
96
Nigeria
94
Africa
92
Tanzania
88
Zambia
85
Rwanda
83
Latin America and the Carribbean
82
Bangladesh
81
Syria
79
Malawi
71
Ukraine
70
Namibia
65
Ghana
59
Philippines
50
Cambodia
42
South Sudan
41
Eastern Europe
41
Zimbabwe
40
Congo, Democratic Republic of
39
Indonesia
39
Guinea
38
South–East Asia Region
36
Asia
36
Mozambique
35
Lesotho
35
Germany
29
Brazil
28
West and Central Africa
27
Russia
27
East and Southern Africa
26
Yemen
24
Haiti
23
Eastern Europe and Central Asia
22
Senegal
21
Middle East and North Africa
20
Afghanistan
18
Botswana
18
Pakistan
17
Burkina Faso
16
Eswatini/ Swaziland
16
Western Pacific Region
16
Vietnam
16
Lebanon
15
Venezuela
15
Cameroon
14
Thailand
14
USA
13
Somalia
13
Colombia
13
Sudan
12
Central African Republic
12
Madagascar
12
Jordan
10
Laos
10
Moldova
10
China
9
Benin
9
Sri Lanka
9
Iraq
8
Turkey
8
Papua New Guinea
7
Palestine
7
Tajikistan
7
Mali
6
Argentina
6
Peru
6
Hungary
6
Chile
6
Poland
6
Albania
6
Romania
6
Jamaica
6
United Kingdom
6
Côte d’Ivoire / Ivory Coast
5
North Macedonia
5
Burundi
5
Greece
5
North America
5
Portugal
5
Chad
4
Libya
4
Angola
4
Paraguay
4
Timor Leste/ East Timor
4
Kyrgyzstan
4
Kazakhstan
4
Guinea-Bissau
3
Egypt
3
Singapore
3
Serbia
3
Croatia
3
Mexico
3
Southern Africa
3
Canada
3
Iran
3
Georgia
3
Japan
3
Mauritius
3
Spain
3
Niger
2
Gambia
2
Honduras
2
Ecuador
2
El Salvador
2
Guatemala
2
Other region
2
Fiji
2
Bhutan
2
Italy
2
Armenia
2
Bulgaria
2
Estonia
2
Lithuania
2
Slovakia
2
Turkmenistan
2
Azerbaijan
2
Belarus
2
Morocco
1
Togo
1
Malaysia
1
Ireland
1
Dominican Republic
1
Switzerland
1
Bolivia
1
Nicaragua
1
Mongolia
1
Congo-Brazzaville
1
Qatar
1
Uzbekistan
1
Denmark
1
France
1
Tunisia
1
Norway
1
Israel
1
Bosnia and Herzegovina
1
Latvia
1
Belize
1
Costa Rica
1
Panama
1
Authors & Publishers
Publication Years
Category
Countries
2123
Clinical Guidelines
423
Key Resources
403
Public Health
367
Women & Child Health
320
Capacity Building
123
Pharmacy & Technologies
39
Annual Report MEDBOX
3
Toolboxes
Mental Health
600
COVID-19
537
HIV
468
Disability
263
Planetary Health
223
Conflict
219
TB
213
NCDs
159
AMR
154
NTDs
154
Caregiver
153
Ebola & Marburg
141
Refugee
138
Global Health Education
103
Rapid Response
95
Pharmacy
86
Health Financing Toolbox
86
Natural Hazards
79
2.0 Rapid Response
58
Malaria
55
Specific Hazards
47
Cholera
31
Zika
31
Polio
30
Social Ethics
26
Typhoon
4
South Sudan
2
Questions & Answers
AMR is one of the Key priority of the global health security agenda action package, as well as it is one of the commitments of Ministry of Public Health Afghanistan to combat AMR. In Afghanistan because of war and some other political issues the borders of the country are not well secured and well c
...
Volunteers are impacted by COVID-19 like everyone else worldwide. They worry about being stigmatized by family and community members, fear contracting the virus, having to be in isolation or quarantine, losing colleagues etc. Volunteers may also be affected by witnessing the death of someone they su
...
As part of the project ‘Equitable health financing for a strong health system in Mozambique’, N’weti and Wemos developed this policy brief with actionable policy recommendations for the Mozambican government and international organizations on how to increase resources for health in a sustainab
...
Comprehensive public health action on population ageing is urgently needed. This will require fundamental shifts, not just in the things we do, but in how we think about ageing itself. The World report on ageing and health outlines a framework for action to foster Healthy Ageing built around the new
...
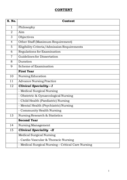
Post Graduate programme is essential to prepare nurses to improve the
quality of nursing education and practice in India. .
Post graduate programme in nursing builds upon and extends competence
acquired at the graduate levels, emphasizes application of relevant theories
into nursing practice, ed
...
This is an update (third edition) of the BACPR Standards & Core Components and represents current evidence-based best practice and a pragmatic overview of the structure and function of Cardiovascular Prevention and Rehabilitation Programmes (CPRPs) in the UK. The previously described seven standards
...
Accessed: 11.03.2019
This document aims to help EU/EEA public health authorities in the tracing and management of persons, including healthcare workers, who had contact with COVID-19 cases. It outlines the key steps of contact tracing, including contact identification, listing and follow-up, in the context of the COVID-
...
Цель данной аналитической записки – предоставить краткое изложение информации и соображений,
касающихся принятия оптимальных мер в отношении гриппа во время па�
...